Permacath Insertion.
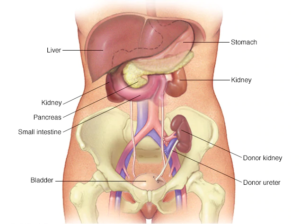
 Dialysis is the lifeline of Chronic Kidney diseases [CKD] / Renal failure
patients. AV Fistual is the most common dialysis access method. If it fails or
can’t be done then Permcath placement is 2nd preferred method of long term
Hemodialysis.
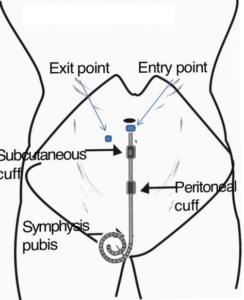
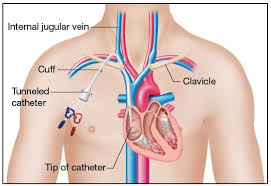
A flexible tube which is inserted into vein having 2 hollow bores is called as
Permcath. Generally Permcath is inserted in internal jugular vein and very
rarely in femoral vein in the groin region. One hollow bore carries blood from
body to dialysis machine whereas the other bore carries blood from dialysis
machine to body. There’s a cuff which holds catheter in place protecting from
infections which also acts like a barrier.
Dialysis is the lifeline of Chronic Kidney diseases [CKD] / Renal failure
patients. AV Fistual is the most common dialysis access method. If it fails or
can’t be done then Permcath placement is 2nd preferred method of long term
Hemodialysis.
A flexible tube which is inserted into vein having 2 hollow bores is called as
Permcath. Generally Permcath is inserted in internal jugular vein and very
rarely in femoral vein in the groin region. One hollow bore carries blood from
body to dialysis machine whereas the other bore carries blood from dialysis
machine to body. There’s a cuff which holds catheter in place protecting from
infections which also acts like a barrier.
BEFORE THE PROCEDURE
1. Patient is kept in NBM for 5-6 hours before the procedure. 2. If the patient is already on blood thinners or any particular medicines or allergic to any medicines, infections in past then the doctor should be reported about the same. 3. Patient should undergo physical examination test, blood tests and colour Doppler test before the procedure.DURING THE PROCEDURE
A flexible tube called as IV Cannula is inserted into back side of the hand inorder to deliver drugs directly into the vein. Patient is asked to lie flat on the bed thereby sedatives are administered intravenously to relax the body and relieve any pain till the procedure is completed. Antiseptic solution or sterile is rubbed at body region wherein catheter is to be inserted. Doctor records oxygen level in the blood. After sedating the patient doctor will guide a wire into the superior venacava or right atrium of heart through internal jugular vein. In this way doctor creates the tunnel and thereby guides the catheter into the right atrium of the heart. Cuff keeps the catheter in place or holds it in place which is present under the chest wall. The region where catheter leaves chest wall is stitched and transparent dressing is applied over the stitched area. Cathlab Imaging tests are conducted after the permcath insertion inorder to confirm the Permcath position. This procedure lasts for approximately 45-50 mins. The advantages of Permcath are like it is less prone to infection and moreover it lasts for much longer duration than jugular catheter.Haemodialysis
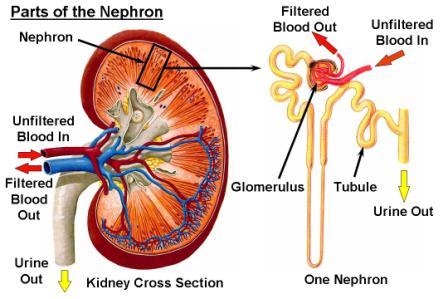
Hemodialysis is a treatment to filter wastes and water from your blood, as your kidneys did when they were healthy. Hemodialysis helps control blood pressure and balance important minerals, such as potassium, sodium, and calcium, in your blood.
Hemodialysis can help you feel better and live longer, but it’s not a cure for kidney failure.
What happens during hemodialysis?
During hemodialysis, your blood goes through a filter, called a dialyzer, outside your body. A dialyzer is sometimes called an “artificial kidney.”
At the start of a hemodialysis treatment, a dialysis nurse or technician places two needles into your arm. You may prefer to put in your own needles after you’re trained by your health care team. A numbing cream or spray can be used if placing the needles bothers you. Each needle is attached to a soft tube connected to the dialysis machine.

The dialysis machine pumps blood through the filter and returns the blood to your body. During the process, the dialysis machine checks your blood pressure and controls how quickly
- blood flows through the filter
- fluid is removed from your body
What happens to my blood while it’s in the filter?
Blood enters at one end of the filter and is forced into many, very thin, hollow fibers. As your blood passes through the hollow fibers, dialysis solution passes in the opposite direction on the outside of the fibers. Waste products from your blood move into the dialysis solution. Filtered blood remains in the hollow fibers and returns to your body.

Your nephrologist—a doctor who specializes in kidney problems—will prescribe a dialysis solution to meet your needs. The dialysis solution contains water and chemicals that are added to safely remove wastes, extra salt, and fluid from your blood. Your doctor can adjust the balance of chemicals in the solution if
- your blood tests show your blood has too much or too little of certain minerals, such as potassium or calcium
- you have problems such as low blood pressure or muscle cramps during dialysis
Can the dialyzer do everything my kidneys once did?
No. Hemodialysis can replace part, but not all, of your kidney function. Dialysis will help improve your energy level, and changes you make to your diet can help you feel better. Limiting how much water and other liquid you drink and take in through foods can help keep too much fluid from building up in your body between treatments. Medicines also help you maintain your health while on dialysis.
Where can I have hemodialysis?
You can receive treatment at a dialysis center or at home. Each location has its pros and cons
Dialysis center
Most people go to a dialysis center for treatment. At the dialysis center, health care professionals set up and help you connect to the dialysis machine. A team of health care workers will be available to help you. You will continue to see your doctor. Other team members may include nurses, health care technicians, a dietitian, and a social worker.
Set schedule
You’ll have a fixed time slot for your treatments, usually three times per week: Monday, Wednesday, and Friday; or Tuesday, Thursday, and Saturday. Each dialysis session lasts about 4 hours. When choosing a dialysis schedule, think about your work and child care or other caregiving duties.
Nighttime option
Some dialysis centers offer nighttime treatments. These treatments occur at the dialysis center 3 nights a week while you sleep, which takes longer. Getting longer overnight dialysis treatments means
- your days are free.
- you have fewer diet changes.
- your liquid allowance (how much liquid you can drink) is closer to normal.
- you may have a better quality of life than with a standard hemodialysis schedule. Longer treatment sessions may reduce your symptoms.
How do I find a dialysis center?
Your doctor, nurse, or social worker can help you find a dialysis center that’s convenient for you. Under Medicare rules, you have the right to choose the dialysis center where you’ll receive treatment. Your doctor will give your medical information to the dialysis center you choose.
Most large cities have more than one dialysis center to choose from. You can visit the centers to see which one best fits your needs. For example, you can ask about a center’s rules for laptop and cellphone use, as well as for having visitors. You may want the center to be close to your home to save travel time. If you live in a rural area, the closest dialysis center may be far from your home. If you’d have a hard time getting to the dialysis center, you may want to consider home dialysis treatments such as home hemodialysis or peritoneal dialysis.
treatments over the internet.
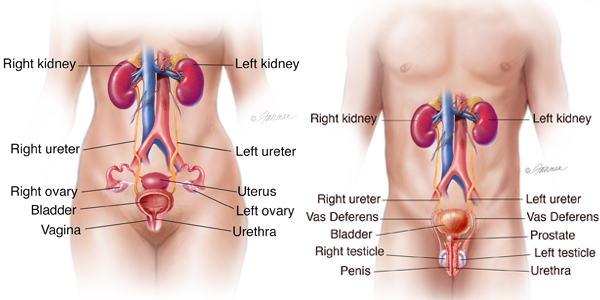
Peritoneal dialysis.
What is peritoneal dialysis and how does it work?
Peritoneal dialysis is a treatment for kidney failure that uses the lining of your abdomen, or belly, to filter your blood inside your body. Health care providers call this lining the peritoneum.
A few weeks before you start peritoneal dialysis, a surgeon places a soft tube, called a catheter, in your belly.
When you start treatment, dialysis solution—water with salt and other additives—flows from a bag through the catheter into your belly. When the bag is empty, you disconnect it and place a cap on your catheter so you can move around and do your normal activities. While the dialysis solution is inside your belly, it absorbs wastes and extra fluid from your body.

After a few hours, the solution and the wastes are drained out of your belly into the empty bag. You can throw away the used solution in a toilet or tub. Then, you start over with a fresh bag of dialysis solution. When the solution is fresh, it absorbs wastes quickly. As time passes, filtering slows. For this reason, you need to repeat the process of emptying the used solution and refilling your belly with fresh solution four to six times every day. This process is called an exchange.
You can do your exchanges during the day, or at night using a machine that pumps the fluid in and out. For the best results, it is important that you perform all of your exchanges as prescribed. Dialysis can help you feel better and live longer, but it is not a cure for kidney failure.
How will I feel when the dialysis solution is inside my belly?
You may feel the same as usual, or you may feel full or bloated. Your belly may enlarge a little. Some people need a larger size of clothing. You shouldn’t feel any pain. Most people look and feel normal despite a belly full of solution.
What are the types of peritoneal dialysis?
You can choose the type of peritoneal dialysis that best fits your life:
- continuous ambulatory peritoneal dialysis (CAPD)
- automated peritoneal dialysis
The main differences between the two types of peritoneal dialysis are
- the schedule of exchanges
- one uses a machine and the other is done by hand
If one type of peritoneal dialysis doesn’t suit you, talk with your doctor about trying the other type.
CAPD doesn’t use a machine. You do the exchanges during the day by hand.
You can do exchanges by hand in any clean, well-lit place. Each exchange takes about 30 to 40 minutes. During an exchange, you can read, talk, watch television, or sleep. With CAPD, you keep the solution in your belly for 4 to 6 hours or more. The time that the dialysis solution is in your belly is called the dwell time. Usually, you change the solution at least four times a day and sleep with solution in your belly at night. You do not have to wake up at night to do an exchange.

Automated peritoneal dialysis. A machine does the exchanges while you sleep.
With automated peritoneal dialysis, a machine called a cycler fills and empties your belly three to five times during the night. In the morning, you begin the day with fresh solution in your belly. You may leave this solution in your belly all day or do one exchange in the middle of the afternoon without the machine. People sometimes call this treatment continuous cycler-assisted peritoneal dialysis or CCPD.
Where can I do peritoneal dialysis?
You can do both CAPD and automated peritoneal dialysis in any clean, private place, including at home, at work, or when travelling.
Before you travel, you can have the manufacturer ship the supplies to where you’re going so they’ll be there when you get there. If you use automated peritoneal dialysis, you’ll have to carry your machine with you or plan to do exchanges by hand while you’re away from home.
How do I prepare for peritoneal dialysis?
Surgery to put in your catheter
Before your first treatment, you will have surgery to place a catheter into your belly. Planning your catheter placement at least 3 weeks before your first exchange can improve treatment success.
Although you can use the catheter for dialysis as soon as it’s in place, the catheter tends to work better when you have 10 to 20 days to heal before starting a full schedule of exchanges.
Your surgeon will make a small cut, often below and a little to the side of your belly button, and then guide the catheter through the slit into your peritoneal cavity. You’ll receive general or local anesthesia, and you may need to stay overnight in the hospital. However, most people can go home after the procedure.